
Lung Flute
Developed by
Medical Acoustics
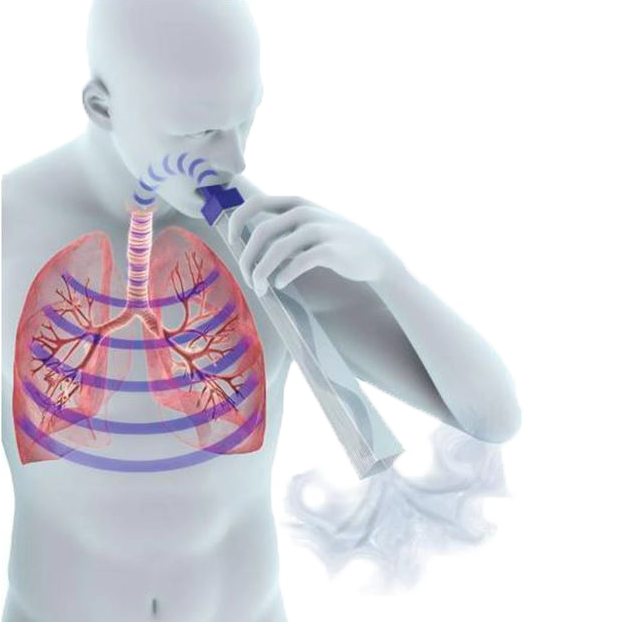
The Lung Flute by Medical Acoustics is the only FDA-cleared product that uses Sound Wave Vibration to stimulate the body’s natural mucus-clearing system – effectively thinning and dislodging mucus deep in the lungs so that it’s easier to cough up. The small, reusable, plastic device is non-invasive, easy to use and drug-free – just blow into the mouthpiece and the device will do the rest.
The Award-winning Lung Flute, is an important part of Bronchial Hygiene Therapy (BHT). BHT can be used for a variety for congestive conditions such as: Chronic Obstructive Pulmonary Disease (COPD), bronchitis, pneumonia, asthma, emphysema or other chronic respiratory ailments.
Clinical tests at the VA hospitals have proven the Lung Flute’s ability to break up mucus in the lungs, making it equally effective for both therapeutic and diagnostic use. Unlike other devices, which rely on pressure and can’t reach deep lung mucus, the Lung Flute’s technology is based on low-frequency acoustic waves that are produced when you blow into the mouthpiece.
EXPAND A LUNG RESEARCH:
BREATHING RESISTANCE EXERCISE
The flow of air in and out of the alveoli is called ventilation and has two stages: inspiration (or inhalation) and expiration (or exhalation). To accomplish this, the whole thorax moves and changes size, due to the action of two sets of muscles: the intercostal muscles and the diaphragm. These are the muscles that are strengthened by using the deep Breathing Resistance Exerciser such as SLB, to enable you to breathe deeper, easier and better.
INSPIRATION (INHALING) WITH RESISTANCE:
The diaphragm contracts and flattens downwards
The external intercostal muscles contract, pulling the ribs up and out
The volume of the thorax increases
More air is delivered deeper into the lungs
The lung and alveoli volume increases
More oxygen is absorbed
EXPIRATION (EXHALING) WITH RESISTANCE:
The abdominal muscles contract, pushing the diaphragm upwards
The internal intercostal muscles contract, pulling the ribs downward
This gives a larger and faster expiration
More CO2 is expulsed
In essence, you inhale more oxygen, and you exhale more carbon dioxide. The result is a substantial improvement in shortness of breath and endurance through better breathing.
All is done naturally, with the help of the SLB Breathing Exerciser.
RESEARCH SUPPORT ATTENTION ALL ATHLETES!!!
Consider Training Your Respiration.
Boutellier U, Buchel R, Kundert A, Spengler C.
Department of Physiology, University of Zurich, Switzerland.
Recently, we have shown that an untrained respiratory system does limit the endurance of submaximal exercise (64% peak oxygen consumption) in normal sedentary subjects. These subjects were able to increase breathing endurance by almost 300% and cycle endurance by 50% after isolated respiratory training. The aim of the present study was to find out if normal, endurance-trained subjects would also benefit from respiratory training. Breathing and cycle endurance, as well as maximal oxygen consumption (VO2max) and anaerobic threshold, were measured in eight subjects. Subsequently, the subjects trained their respiratory muscles for 4 weeks by breathing 85-160 1 min.-1 for 30 min daily. Otherwise, they continued their habitual endurance training. After respiratory training, the performance tests made at the beginning of the study were repeated. Respiratory training increased breathing endurance from 6.1 (SD 1.8) min to about 40 min. Cycle endurance at the anaerobic threshold [77 (SD 6) %VO2max] was improved from 22.8 (SD 8.3) min to 31.5 (SD 12.6) min while VO2max and the anaerobic threshold remained essentially the same. Therefore, the endurance of respiratory muscles can be improved remarkably even in trained subjects. Respiratory muscle fatigue induced hyperventilation which limited cycle performance at the anaerobic threshold. After respiratory training, minute ventilation for a given exercise intensity was reduced and cycle performance at the anaerobic threshold was prolonged.
In Summary, the condition of the respiratory system is more important for endurance exercise performance of healthy trained subjects than hitherto assumed. Not only do respiratory muscles fatigue during intense endurance exercise, but prefatigued respiratory muscles can also impair performance. In turn, respiratory resistance training can improve endurance exercise performance.
IMPROVE ENDURANCE AND PERFORMANCE THROUGH RESPIRATORY MUSCLE TRAINING
Claes E.G. Lundgren, M.D., PhD., professor of physiology and Biophysics in the State University of New York, UB School of Medicine. This research was supported by the US Navy Experimental Diving Unit. In this pioneering work, subjects who followed breathing resistance training improved their snorkel surface swimming time by 33% and their underwater Scuba swimming time by 66%.
“The above data is in agreement with previous studies in cyclist, rowers, and runners. They suggest that athletes in most sports could improve their performance by undergoing respiratory muscle training. It is also clear that the greater the stress on the respiratory system, the larger the improvement in performance.”
During high-intensity exercise, when the breathing muscles become fatigued, the body switches to survival mode and “steals” blood flow and oxygen away from locomotor muscles. As a result, these locomotor muscles become fatigued and performance can suffer significantly. Increasing the strength of the respiratory muscles through breathing resistance exercise can prevent this fatigue during sustained exercise situations. The end result is better endurance performance!
-ARTICLE BY : GINA DEMILLO WAGNER – (RUNNER’S WORLD MAGAZINE)
“Runners think about training their heart and legs, but they rarely think about training their lungs,” says Mindy Solkin, owner and head coach of The Running Center in New York City. “A strong respiratory system can improve your running. It’s a simple equation: Better breathing equals more oxygen for your muscles, and that equals more endurance.”
This was backed up by researchers from the Centre for Sports Medicine and Human Performance at Brunel University in England, who recently measured fatigue levels of marathoners’ respiratory muscles and leg muscles. They found a direct link. Runners whose breathing was the most strained showed the most leg weakness and concluded in their study that the harder the respiratory muscles had to work, the more the legs would struggle in a race.
– ARTICLE BY: JOHN HOWARD – (TRIATHLETE MAGAZINE)
” When training only your respiratory muscles, the diaphragm, and intercostals, you will increase both lung strength and capacity, which translates into increased oxygen uptake without beating up the rest of the body.”
“One of the most impressive benefits of correct breathing is the profound relaxation it brings on, meaning it allows the athlete to maintain a high work rate while remaining calm and comfortable.”

I. Therapeutic Clinical Trials

II - Diagnostic Clinical Trials